Roughly 50% of children with CP have a defined perinatal risk factor and roughly 40% of the total number have Hemiplegia.1 Children with hemiplegia have damage on one side of the brain that produces the signs of cerebral palsy on the opposite side of the body. However, the risk factors that cause brain damage produces different patterns of cerebral palsy in babies born early when compared to babies at or near their expected date of delivery. The image shows the different patterns of hemiplegic cerebral palsy in premature compared to full-term babies.
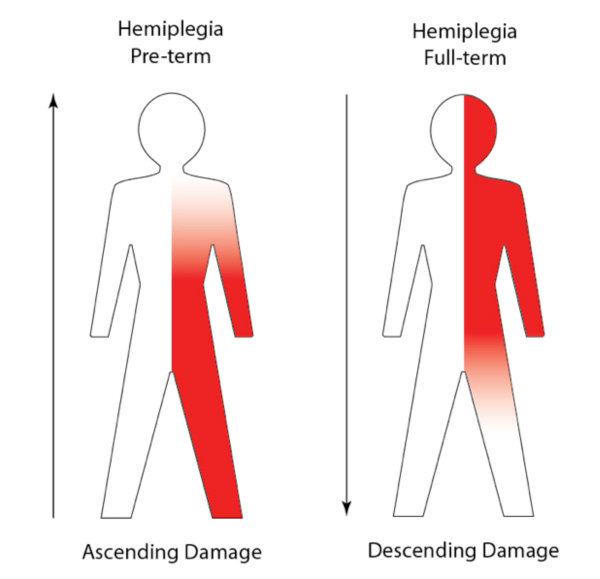
In the baby born early, this damage affects the periventricular white matter of the brain. Either Periventricular Leukomalacia (PVL) or a Grade IV hemorrhage can produce a hemiplegic pattern. Both lesions affect the fiber tracts that control the foot and leg in an ascending pattern. In simple terms, in a preterm infant with hemiplegia, the leg is always more affected than the arm and hand. Speech and cognition are not affected by this localized brain damage.
In the full-term infant, there are two types of unilateral brain lesions. The most common is a Hypoxic-Ischemic Encephalopathy or HIE in a watershed area of the gray matter between the anterior and middle cerebral arteries. The second most common type of damage is a middle cerebral artery stroke.
Hypoxic Ischemic Encephalopathy [HIE] or Neonatal Encephalopathy [NE]?
In both these situations, the site of damage primarily affects the upper limb girdle, hand and face. Speech can also be affected. The pattern of hemiplegia produced by either of these full-term lesions is a descending one with the upper limb and hand more affected than the leg.
Children with either type of hemiplegia will walk. In the CP registry studies reported by Iona Novak1, 99% of children with hemiplegia were walking independently or with an aid. They were scored at GMFCS Levels I to III. The data was not analyzed by birth weight or gestational age, but in my experience, the children with preterm pattern hemiplegia have to work harder to get up and moving and it is really important to keep the foot, ankle and leg in alignment as they grow. The full term child has fewer problems with the leg.
The situation is reversed for functional hand use. The preterm child has fewer problems, especially if the wrist and thumb are maintained in good position. The full term infant tends to have a tighter hand that is less useful and a hand that is not useful becomes a neglected hand. In my experience, most of the full term children will need a wrist and thumb splint early and until they either stop growing or develop functional use. This study demonstrates the importance of a stable wrist and thumb for functional use.
Quick Fixes for 2014 – Stabilize the Wrist and Thumb
In spite of this reality, most children with hemiplegia either do not have a splint or they do not use them consistently. In my opinion, this is a big mistake. As the study above demonstrates, using an appropriate splint results in instantaneous improvement.
What about the other types of CP? Diplegia is a preterm problem and they all have an ascending pattern of involvement.
Spastic Diplegia – Cure For Some, Improvement For All
Quadriplegia can be either preterm pattern or full term pattern and the same rules apply. Preterm quadriplegia pattern is ascending and full term pattern is descending.
Why is this important?
If you know the pattern, you can focus your attention where it is most needed. Parents of a child with cerebral palsy have a lot of competing demands and only a finite amount of time. The good news is that there are now a large number of evidence based and promising best practice interventions that may help. The bad news is that you and your therapy team will have to make choices.1,2 Setting priorities helps. Putting on an AFO and a Wrist/Thumb splint takes 10 minutes at most, but the child benefits from these 10 minutes all day long.
Constraint Induced Movement Therapy (CIMT) is one of the “Gold Standard”, proven interventions that work to improve hand use in children with Hemiplegia. 2
When Does Treatment Stop Being Research?
Now that this technique has passed the single intervention randomized controlled trial phase, it should be obvious that CIMT will work even better if the hand is held in proper alignment. Obvious, but hard to find! I spent half a day looking for an image of a child doing CIMT with good hand alignment.
Neuroplasticity and Hands: Doing The Right Thing, At The Right Time, and In The Right Order
There are lots of images on the Internet of hands in poor alignment with the wrist held in flexion. Human Body Biomechanics 101…When the wrist is in flexion, the grasp strength is weak.
It is time to maximize the results from our interventions and that means we HAVE TO pay attention to alignment and start from the basic biomechanical realities that apply equally to world-class athletes and to children with cerebral palsy. Stabilize the most affected joints first.
As ever, your comments and questions are welcome.
- Iona Novak. Evidence-Based Diagnosis, Health Care and Rehabilitation for Children With Cerebral Palsy. Journal of Child Neurology 2014, 29:1141-1156
- Iona Novak, Sarah McIntyre, Catherine Morgan, Lanie Campbell, Leigha Dark, Natalie Morton, Elise Stumbles, Salli-Ann Wilson, Shona Goldsmith. A systematic review of interventions for children with cerebral palsy: state of the evidence. Developmental Medicine & Child Neurology 2013, 55: 885–910
http://onlinelibrary.wiley.com/journal/10.1111/(ISSN)1469-8749
My daughter was full-term, suffered a pre-natal stroke. Not a true fit into the two cases presented. How to you account for babies like my daughter? CHASA is a good site to look at for including pre-natal stroke victims. My daughter has more issues with her legs than her arms – in fact, no issues with her arm on her weak side. Just leg, foot, and ankle with global balance issues.
Thank you for your comment. You bring up a helpful point. Pre-natal stroke tends to follow the preterm hemiplegia pattern. What pattern you get depends on the maturity of the brain at the time of insult. Pathologically, the most actively growing areas are the most vulnerable. For the baby in the uterus or the same maturity baby who is born prematurely, the result is similar. Equally, I have said that diplegia is most commonly found in babies born prematurely….but some have damage while in the uterus and develop “preterm diplegia” even though they are born at term. Your daughter fits a preterm pattern with the leg most involved. Hope this is helpful.
It is “never” a good idea to use extreme words like, “always”, as in “In simple terms, in a preterm infant with hemiplegia, the leg is always more affected than the arm and hand.” Many kids with hemiplegia in our group, including my own, were pre-term babies, but whose upper extremity is more affected than the lower.
Thank you Lisa, truly, timing is everything, even when describing patterns of damage. This blog is about the relationship of pathologic change in the baby brain and the pattern of CP that results. I stand firm that the leg is more involved in a preterm infant with hemiplegia, but I should have qualified my blanket statement to say “at the start” or “in the early years”. All children with hemiplegia…except for 1% or so with additional complications…do walk and most eventually walk fairly well. It often takes more work with the full term pattern, but those children also walk.
The arm and hand use is not quite so straightforward.One of the most significant confounders is whether the affected side was the genetically programmed dominant hand. For example, in both baby and adult stroke, the right lesion affecting the left hand tends to have more difficulty in recovery.Another factor is that as the children get older, they “chose” not to use the affected hand and thus they lose ground.
The work with CIMT shows that if the hand can grasp, it will improve rapidly with 3-6 weeks of intensive use. Depending on the severity, more than one intensive period may be needed to maintain and build on the new function. The rapid change seen is often too fast for actual growth of new pathways. The most plausible explanation is that the short intensives “unmask” latent pathways that the child had learned not to use. The term for this is “learned non-use”. The take away message is that hand function can improve with several different interventions, but it seems that intensive training is needed to get neuroplastic change. Hope this clarifies my post and thank you again for your comment.
My 23 year old daughter fits with your research- from a cat scan we know she had a stroke between the first and second trimester. She has much more involvement in her hand than foot/leg, but we had bilateral femoral derotations so we don’t really know what life would be like if we hadn’t. I find your research fascinating. I would love to hear more about CIMT- is it useful in adults?
Thank you for your comment. It is fascinating how much knowledge is coming forth from brain scanning. Very early insults between the first and second trimester have a different cause than the stokes that occur in the perinatal period and the losses may be more specific. There is an excellent, if costly book about CIMT in Pediatrics.
Handbook of Pediatric Constraint-Induced Movement Therapy (CIMT): A Guide for Occupational Therapy and Health… by Sharon Landesman Ramey, Patty Coker-Bolt and Stephanie C. DeLuca (Sep 6, 2013)
Members of the AOTA can get it at a significant discount. I urge all parents to let their therapist know about the handbook and to encourage them to get and use it.
Very good informative discussion, I agree the ascending and descending pattern…
My daughter is 6yrs old, she was born full term. At the age of 16months, she was diagnosed with periventricular nodular heterotopia, as a result, she has hemiplegia on her right side…this only affected her leg. How is that possible if full term are “always” affected in the arm and hands more?
Good question. Your child’s problem is one that occurs early in gestation, before birth. The key point is that the pattern is usually determined by the timing of the insult to the brain. So, if the insult occurs in the preterm period, the result is a preterm pattern. If the insult is in a more mature brain, then the result is a full term pattern.Recognizing the different presentations helps us focus our attention concerning therapy.
I have to say I find this article frustrating. I have a son with CP. He is a surviving twin who was born at 27 weeks. He had evidence of PVL and possible head bleed. His twin had the highest level of head bleed measurable and passed away at 3 1/2 days due to pulmonary hemorrhage. My survivor is double hemi or quad depending on who you talk to. His arms are far more involved than his legs; he has limited trunk stability and cannot walk unaided. He also has significant cognitive impairment and Asperger’s-like tendencies when it comes to issues of perseveration, scripting, lack of eye contact, and lack of empathy.
I was looking for information when I clicked through to this article. What I found was a series of generalizations that certainly do not apply to my son and his situation. Is there some difference in outcome because of the multiple birth? Due to extreme prematurity and extreme low birthweight (my boys were 1lb 1oz and 1lb 12oz at birth)?
My mother, an occupational therapist, told me years ago that CP is a garbage bucket term that lumps a plethora of issues under the same diagnosis. Our pediatrician told me, “We are kindergartners when it comes to understanding the brain.” I realize that further understanding of what happened with my sons at or before birth won’t change the outcome, but I find the generalizations and use of definitives like “always” and “never” unhelpful.
In reply to M. Rempel….Thank you for your thoughtful comment. I agree with your mother, the occupational therapist, that CP is a garbage bucket term. The definition includes every type of injury (PVL,IVH,HIE, trauma), hydrocephalus, infection (intrauterine or later occurring), malformation or genetic event that damages the brain of child from conception to 2 years of age. There is no generalization that is wider! Roughly 50% of children have a perinatal risk factor and following these children in an NICU Follow-Up Program allowed me to understand the different ascending and descending patterns of CP. If the brain pathology is typical – white matter in the prematures and grey matter in the full terms, the majority of children will follow the patterns described. I believe it is valuable to know what to expect as it allows the physician to also recognize when the presentation is atypical.
Your son’s condition is very complicated with several risk factors likely contributing to his particular presentation.Extreme prematurity and multiple birth are associated with the scan abnormalities you describe.His CP presentation is complicated and frankly, I do not understand the benefit of differentiating a child with a double hemi from a quadriplegic pattern.To me, the key point is that he has 4 limb involvement. Therapy for this would start with some trunk support.The cognitive issues and Asperger’s like symptoms are not part of the “usual” CP pattern and warrant specific treatments that are separate from the cerebral palsy symptoms. There are several valuable interventions for children on the Autism Spectrum that are not usually available from a therapist working primarily with CP.
All of this is extremely frustrating for the parent trying to find the best possible outcome for their child. Before I retired from clinical practice, I found a later MRI scan helpful in complicated situations like you describe for your son. The MRI can give a detailed view of what is wrong and also what is right about a brain. Knowing what you have to work with can be very helpful to your therapy team.
Hi karen…most of your blogs are exactly matching my son problems. From your blogs i have learnt the techincal terms and issues to discuss with therapists. Every time i will be waiting for your next blog sothat i can see lot more information which will be helpful for many parents. Good Blog.
My son is a 24wker. He had a IVH grade 3 & 4. We were told after this was discovered that he would probably have CP. But this was never mentioned to us since, so I thought he didn’t, especially when they decided that the MRI they had planned to do when he reached age 1 was deemed not necessary; but above you describe CP as a blanket term so does my son have mild CP? 2 years ago at age 3 he had an MRI. They say he has no significant motor deficit. The MRI showed mild bilateral peri ventricular lucamalacia. “He has a mild tightness distally in his lower left limb, there is physical correlate for this. The scan also demonstrated thinning of the corpus callosum, particularly on the posterior aspect.” He attends physio since he was 1, it’s only a couple of checks a year now;and has seen orthotics, braces , insoles, tight X-rays, Botox have all been discussed but all they ever do is give me stretches to do which have never made any difference and he finds painful. There is never any discussion on his diagnosis or prognosis. There doesn’t appear to any issue with his hand. I feel we are missing the window of opportunity to make improvements. What should I be asking or asking for, I would really appreciate any advice.
Dear Helenet, Thank you for your question and I apologize for the delay in responding.He has recovered well from the Grade 3&4 bleeds. The most common problem from a Grade 3 bleed is hydrocephalus and he did not get that! Of the babies with a Grade 4 extension into the white matter, 30-50% recover. Unfortunately, these “Outliers” have not been systematically studied to find out why some do recover completely and others do not. Your son was one of the lucky ones. The mild tightness in the left leg seems to be it. He might qualify as a very mild GMFCS I with a diagnosis of left monoplegia, but it is hard to say without examining him. The key question is whether for not he has any functional limitations. There is a tendency in many areas to consider a child like yours as “good enough”. I look at it differently. I would want him to be balanced. Often there is more issues as they grow, so I would ask the therapy group for help, even though his problem is mild. For the stretches, try warming the muscles up before you stretch….a warm bath or quiet time with a heating pad before the stretch can work wonders.
daughter was 30-weeker with white matter damage. Her hands are more affected than her legs. She can, with a walker, walk in a reciprocal pattern but struggles to bring her hands to midline. Also, her bleed was much larger on the right side so they told us her left side would be more affected. While her left hand is more prone to being fisted she actually has much more functional use of her left side. For that reason, I’m a little wary of predictions made based on imaging. There just seem to be so many variables. So many parents I know have found that not to be the case. My friend’s son was a term infant with damage and they told her he may never suck and swallow when in fact he is considered “Level 1” on gmfcs, so his cp is quite mild. As for autism not being part of the CP patten, isn’t there a higher rate of autism among preterm infants?
Dear Hilary, good questions.You are right to be wary of predictions based on imaging. Unfortunately they are the best we have at this point in time. The baby brain has a remarkable ability to recover…there is much more neuroplasticity in the young brain.That said, in your child, a later scan might help sort out what is happening now. The difficulty you describe in bringing her hands to the midline is unusual and I would ask your doctors if there is anything else going on.
Autism is not part of CP. There are many issues that are considered co-morbidities because they also occur in small babies. RLF and some forms of hearing loss occur more often in preterm babies. But the damage causing these problems is different than the damage causing CP. There have been a few reports of an increased incidence of autism in preterm infants, but the studies are small and not completely convincing. In the 1970’s through to the late 1980’s, I saw literally thousands of preterm babies at the Hospital for Sick Children in Toronto. We followed all babies <1500gm and all had an independent test by a neuropsychologist.In all that time, I saw one child with autism. Since those days, the rates of autism have risen dramatically and so I am not surprised that there are ex-prematures that also have autism. But, it is a different problem, affecting different areas of the brain and most importantly, has different treatments available that may help. My concept of patterns is an attempt to get more specific and away from the garbage bag definition of CP. Hope this helps.
This is interesting, thank you. I was wondering how to judge which side is most affected wit ours. I know this seems like an obvious question, although I feel as though our 3y/o daughter (who survived a perinatal left MCA stroke) has much of her RUE and RLE affected. She can walk but turns her right foot in with the heal elevated. Her right arm/palm is now a helper but she cannot grasp very much yet. Both are very tight and weak. I suppose our focus involves both limbs quite a bit at this point -braces BLE, RUE, rotation straps for BLE, botox both ext, constraint therapy cast, aggressive PT,OT,ST, plus her seizure meds really help to relax her muscles as well. There is some concern that we are asking too much of her, but on the other hand we want the very best outcome for her as well. So should we be more focused and aggressive with 1 extremity at a time at this point? Would that help her success overall? If so, in your opinion, should our focus should be more so on her RUE or RLE 1st?
Hi Nina,
I apologize for the delay in responding.I think you are doing a terrific job. I know it seems like it is too much at times, but the first 4-6 years are the really important ones to do the most. At this young age, I suggest you continue to work with everything and see how her brain recovers. You are doing a good job keeping her alignment and treating spasticity. This is really important in the first years as the growth rate is so rapid. Don’t get discouraged.We know that 99% of children with hemiplegia walk and overall most score on the GMFCS at Level I, II, or III…mild to moderate severity.As long as you keep up with the Botox as needed and the AFO, you can be reasonably sure that the walking skills will improve with time. It is harder to encourage hand use so I would focus on it more.
Hope this helps,Karen
My son has cerebral palsy and we were also told he has no white matter on right side of brain. What does that mean?
Dear Tonya,please read these 2 blog posts about cerebral palsy with a one-sided brain problem like no white matter on one side.
http://www.karenpapemd.com/cerebral-palsy-hemiplegia-gmfcs-i-to-iii-part-one/
http://www.karenpapemd.com/cerebral-palsy-hemiplegia-gmfcs-i-to-iii-part-two/
The type of cerebral palsy is most often a hemiplegia, affecting the opposite side of the body to the brain lesion. I would ask your doctor to explain this to you.Hope this helps.
Hi Karen,
My son was born just short of 12 weeks premature. He had normal apgar scores and I was told everything was OK he had brain scans and I was told these were normal.
At the age of 2 and a half he was diagnosed with diaplegic cp. In 2016 at the age of ten he was sent for an Mri and it revealed a subarachnoid cyst in the right middle fossa. After these findings I decided to query what has happened to my son.
The ultra sound scans from when he was 2 days old were brought up and the consultant said that they showed cystic pvl and that the scans should never have been marked as normal.
I was told in 2012 that he was no longer diaplegic as he was more hemiperatic in appearance, so had diagnosis of left sided hemi paresis.
Could you shed any light on this as I’ve asked if the cystic pvl is now the cyst that he has in the right side of his brain and is it this that has caused his left sided hemi paresis. Also how could this have happened. The replies I get are what does it matter now anyway. Would love to be enlightened if possible.
Kind regards
Thank you for your email. The sequence of reports on your child scans are confusing. I would ask for their official report and see if it makes more sense when you read those through. It you really want to get to the bottom of what went on, I would look for a good neurologist to review all the scans. I think it most likely that the right-sided cyst is causing the left-sided hemiparesis. I hope this helps.