Most children and adults with Cerebral Palsy (CP) and Brachial Plexus Injury (BPI) live with chronic pain. The more severe the injury, the earlier the pain onset.
I went looking for a good infographic on childhood pain and could not find one. There are hundreds available for the wide variety of chronic pain syndromes in adults, but the childhood ones seem to be limited to chronic abdominal pain and cancer management. There is a lot of information available for adult neck, back, joint and myofascial pain, but very little with a pediatric focus.
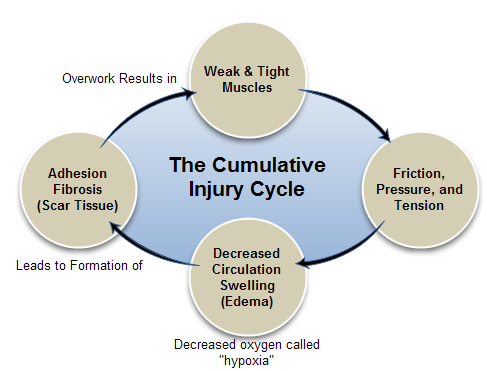
I picked this infographic because it deals with normal, healthy muscle that is overworked for a variety of reasons. Children with CP start with weak and tight muscles when they wake up. These are the realities. There have been lots of studies that document muscle weakness and overwork in patients with CP. Spastic muscle are tight. In BPI, the weak, poorly innervated muscles do not support the arm well and other muscles in the neck, and back are overworked attempting to compensate. Over time, they also become tight causing scarring, adhesions and “trigger points”.
My last post on pain sparked many comments and questions, mainly concerning how to know whether or not the child is in pain. (How Much Does It Hurt) Babies tell us if they are in pain. Every parent soon learns that “gas” causes pain in babies that is relieved by a burp. Fortunately, musculoskeletal pain at this age is very rare, mostly seen in infants and toddlers with the most severe forms of spasticity. If you think your child has this severe type of pain, you should discuss it with your doctor.
Most pain in the early years of life with CP are caused by gastroesophageal reflux disease, constipation or hip dislocation. All of these conditions can cause noticeable pain. It is usually episodic and you can link it to body position as in reflux or change in position when you move a painful joint. Again, your physician can help you diagnose and treat these conditions.
Chronic musculoskeletal pain starts with a muscle pain cycle as described in the infographic above. As I explained in the previous pain post, young and/or non-verbal children cannot easily identify “pain”. However, some non-verbal children can use the type of pain scale chart I put in the previous post. (How Much Does It Hurt) The non-verbal signs of a possible pain problem are fatigue, sleep problems, and cognitive or mood disturbances. If parents watch the younger child carefully, thinking about the question of pain, it starts to become clear that some events are associated with pain. For example, if a child settles back to sleep after a position adjustment, pain is the probable cause of waking.
In the older child, teen or adult who can identify pain, a pain history is important.
When did it start?
How much does it hurt?
Where does it hurt?
How does it vary through the day and night?
What helps and what makes it worse?
Another question was whether children with CP or BPI have a higher than normal pain tolerance. I have not seen any evidence of this, but it would be a useful study to do in teens and older adults. My experience is that children develop coping mechanisms to deal with the reality of chronic pain. As the boy with BPI said, “It always hurts. No point in complaining until it really hurts.” Or the young boy with Clubfoot saying, “I didn’t know it hurt until it stopped.” If a child lives with a chronic, low level of pain, small “hurts” do not get the same response as with a normally pain-free child. In a sense, they have habituated to a baseline level of pain and only respond when a new pain exceeds that threshold.
If you have ever asked for a neck rub or relaxed in a hot tub after physical labor, you know what a stiff, sore muscle feels like. I strongly suggest a massage appointment for parents of a child with a motor problem if you have not experienced it. My point is that if you recognize what a relaxed muscle feels like, you are more likely to provide the same for your child. I have sent teens to have a massage and the most common response I get back is, “I never knew my legs could feel like that!”
This is part of a comment from Liz Ruork, a massage therapist/friend of mine in Toronto.
“A massage therapist is a great place to look for help with pain. In the United States, the individual States vary a great deal when it comes to education, regulation and organization of Massage Therapists. However, there is a national organizing body, the American Massage Therapy Association, where you can find a Massage Therapist by location. Here is a link for the AMTA.
There are many Massage Therapists who have training and experience with Cerebral Palsy and other Neuro-motor conditions. You may want to check with local support groups. A good Massage Therapist will not only treat your child, but also teach you techniques that help you to understand and manage his pain better yourself.
In the meantime, please use Karen’s suggestion about warmth. I recommend an electric mattress pad designed to heat the whole bed very gently. You can easily put it on a timer to give your child about 30 minutes of heat both at bedtime and before waking up. Electric mattress pads are available from retailers like J.C. Penny, Bed Bath and Beyond and many others.”
In many cases, pain is diagnosed by a behavioral change when it is treated. Start with warmth and gentle massage of your child’s tight muscle in one limb. See for yourself that the child is more relaxed. Look again at the infographic. It shows what happens to a weak or tight muscle left untreated.
Further Reading
How the American Pain Society describes chronic childhood pain. http://www.americanpainsociety.org/uploads/pdfs/aps12-pcp.pdf
Poor Alignment Equals Chronic Pain
Setting and Achieving Goals – A Family Perspective
Muscle Imbalance Hurts Growing Bodies
Spasticity is a Body and Brain Habit
Take The Mystery Out Of Stretching