The boy on the left with a ball is wearing a set of standard issue AFO’s that block the spastic tendency to plantar flex at the ankle. The boy on the right has a new type of support that creates optimum weight bearing. Do you see the difference in their body posture?
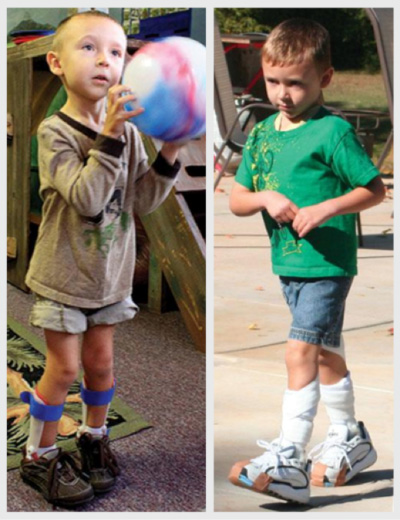 The boy on the left has his feet held flat, but he is flexed at the knees and hips with a compensatory lordosis in his low back. His tone is “overflowing” into his hands, arms, shoulders and even his neck. The child on the right has a normal posture and a heel-toe gait
The boy on the left has his feet held flat, but he is flexed at the knees and hips with a compensatory lordosis in his low back. His tone is “overflowing” into his hands, arms, shoulders and even his neck. The child on the right has a normal posture and a heel-toe gait
This link is to an article by Billi Cusick, PT that explains the New Paradigm is some detail. I strongly recommend that parents share this exciting article with their therapists, orthotic specialist and physicians.
In this series of posts, I have argued that much of what we clinically call “spasticity” is actually a learned body habit. (Spasticity is a Body and Brain Habit) The brain injury causing cerebral palsy is non-progressive, yet the major problem of spasticity is progressive. The spasticity or tone gets worse as the child moves against gravity and as they grow. Tone is dramatically improved when the child has surgical orthopedic realignment of the legs. The tone decreases with proper body alignment. This implies that spasticity is, in part, a learned body habit that is magnified and perpetuated by body mal-alignment. The question is whether earlier, proper alignment, as in the boy on the right, will prevent some of the known problems with growth. Unfortunately, regular AFO’s do not necessarily improve the amount of resting tone in the leg. There is now some research that is supporting a new way of thinking about increased tone at the ankle that leads to an equinus deformity of the ankle.
When I first heard about this new paradigm, I frankly thought it was crazy. I had been taught that having a child up on the toes was the problem and the solution was to fit them with either a solid or articulated AFO that kept the ankle in neutral. Plantar flexion or toe walking was the problem and the solution was to keep the foot flat. In truth, this was rarely a satisfactory solution as the heel was often pulled up inside the AFO and the tension between the upward pull of the gastrocnemius muscles at the back of the leg and the resistant brace often resulted in a pronated foot. The conflict between the rigid brace and the tendency of the foot to plantar flex also led to skin irritations and discomfort. All of these factors combined to keep the child in an anatomically and biomechanically incorrect posture as seen in the boy on the left.
The new paradigm, explained to me by Elaine Owen and Billi Cusick, approaches the problem from a completely different viewpoint. Rather than looking at the length of the gastrocnemius muscles, they have looked at the reality that when a child is moving forward in a plantar flexed position, the body weight is incorrectly distributed. The goal of any intervention is to get the child weight bearing through their heel, allowing for a more balanced response throughout the body. This is accomplished by building up a wedge under the heel to support it in its regular resting position. This has an almost immediate effect of allowing the child to weight bear through the heel, not the toe. Once there is a stable platform, the child can practice weight shifts and gradually incorporate this key skill that is a necessary prerequisite for walking independently.
Billi recently did a course on this new paradigm at the Hospital for Sick Children in Toronto. There is now a strong cohort of up-to-date trained therapists and orthotists. This method is new and like all new methods, there is some initial resistance. Now that I am over my first response and have seen some very good results, I am very happy to bring the information forward to you.
For more information about courses for therapists and orthotists, visit http://www.gaitways.com/courses For information about already trained people for these orthotics and/or TheraTogs, you can contact Jean at admin@gaitways.com
Remember, the goal of any support option is to ensure that the child learns to walk in the best possible way. (When Will My Child Walk?) Weakness, spasticity and poor balance are the key problems that interfere with the development of walking skills. Muscle weakness is universal in children with early neurologic injuries and spasticity complicates the problems for many of them. (What About Spasticity?) Daily stretching and massage should start in infancy and continue throughout the growing period. IF the child’s muscles are always stiff, they will never learn to relax them. (Muscle Imbalance Hurts Growing Bodies) Once the baby starts to move against gravity, spasticity will increase. It also increases with every growth spurt. (Spasticity is a Brain and Body Habit) It is always easier to prevent a bad habit than it is to change an established one. Talk to your therapist and physician about core support and foot/ankle stability. (First the Trunk, Then the Ankle – Spasticity #5) Remember, whatever the body does, it learns to do better. Great alignment is the first step to keeping them from just “Learning to do Bad Better”.
I look forward to your comments and/or questions.
I am wondering if there is a way to have our daughter evaluated by a therapist for this? We struggle so much with her AFO’s ans they never work for her. Is there a list of providers who could evaluate her?
Thanks!
Kristin, sorry for the delay in responding. If you contact jbrown@theratogs.com she might be able to track down a list of the people that have been trained at one of Billi Cusick’s courses on the new paradigm. Karen
At what age should we try the new afo? My grand son is 25 monthes not walking yet
I suggest you print the post and ask your therapist and physician this question. If he is standing, then it is important to make sure he has a stable base of support and that usually means an AFO. That said, every child is different and it is important to check with your own team.
Hi Karen, my name is Liane Norman, I recently discovered your website and blog and relishing the information you put out there. I am a physiotherapist in Ottawa and certified Theratogs fitter and also took Billi’s course on this new paradigm. I don’t do casting but work with an orthotist here in Ottawa who was at Billi’s course and does the castings and will build up wedges for my little patients. I co-own Pediatric Physio and Occupational Therapy with an occupational therapist.
Thank you Liane. It is sometimes hard to identify up-to -date therapy programs and I appreciate this information.I always surprised by the resistance to new ideas. Thank you for pushing forward towards a better future for the children.Karen
My son is 25 years old. He has worn AFO’s since he was 4 or so. The staff at his supportive community living have told me that “a doctor” told them that he needs to wear the AFOs every day all day. I have always had him go without them on weekends, and weekday evenings, in the interest of allowing all his muscles to develop. Does he even need to wear them anymore? Am I wrong in saying that he needs walking time without AFO’s on? His gait is not significantly different with or without AFO’s. I think he “clomps” more with the AFO’s on–but not in a very significant way. What do y’all think?
I would have hime re-evaluated by a good orthopedic surgeon.Your story is rare. Most teenagers discard their AFO’s. Once they stop growing….and your son has…then the need is less. An in-shoe orthotic may be all he needs